The World Health Organization has identified remote patient monitoring as one of the healthcare delivery models with the potential to significantly improve global health outcomes.
What began as a chronic-disease management tool is now evolving into infrastructure, embedded across workplaces, campuses, homes, offshore sites, and even cruise vessels.
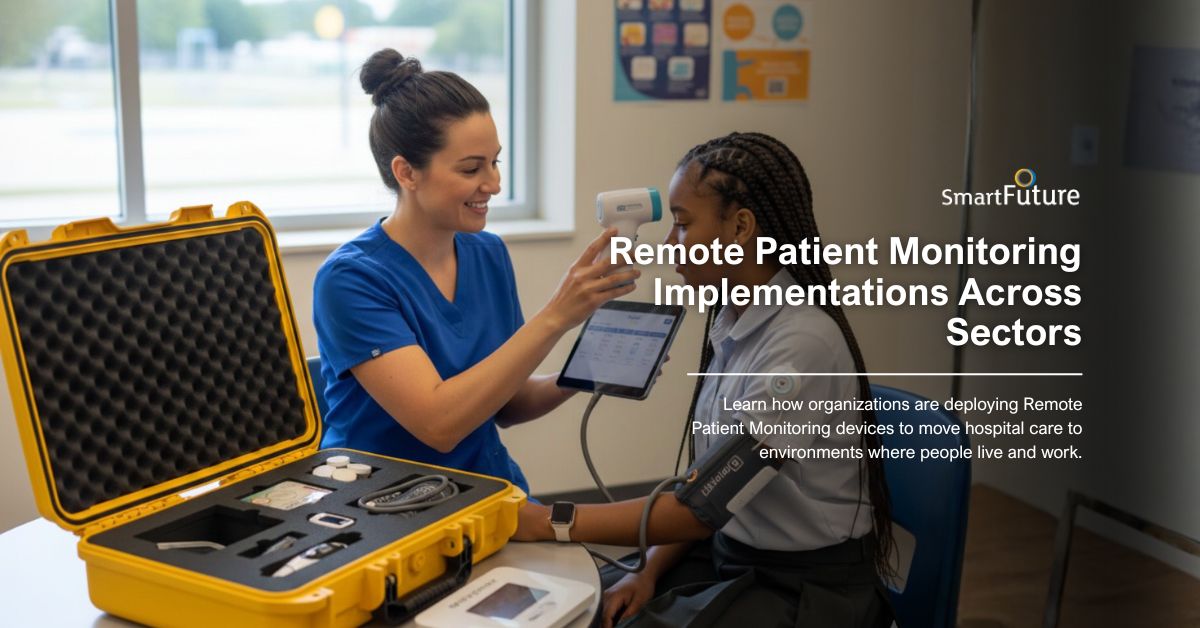
From industrial safety to elderly care, organizations are deploying connected medical devices to move care beyond hospitals and into the environments where people live and work.
Below are nine real-world remote patient monitoring examples reshaping healthcare delivery by location.
Educational institutions are increasingly responsible for managing chronic conditions such as asthma, diabetes, and epilepsy among students. School nurses cannot be everywhere at once.
Remote patient monitoring allows schools to deploy connected devices, such as glucometers and pulse oximeters, that securely transmit readings to healthcare providers or designated administrators. In larger districts, centralized dashboards enable early intervention before a condition escalates.
In post-pandemic education environments, RPM also supports temperature and respiratory monitoring during outbreaks, helping administrators respond to trends instead of isolated incidents.
Impact:
The modern workplace is increasingly tied to health outcomes. Employers managing distributed teams are using remote patient monitoring solutions to support hypertension management, metabolic health, and stress monitoring.
Wearables and connected blood pressure monitors allow HR-linked wellness programs to monitor aggregate trends while preserving individual privacy. For employees with chronic conditions, providers can monitor adherence and adjust treatment plans without requiring time off for clinic visits.
The shift is particularly pronounced in countries facing clinician shortages, where virtual care flexibility is becoming a permanent policy.
Impact:
As aging populations expand, long-term care facilities face resource constraints. Remote patient monitoring devices provide continuous visibility into residents’ vitals, reducing reliance on manual checks.
Smart blood pressure cuffs, fall-detection wearables, and connected weight scales allow caregivers to detect deterioration early. In high-risk populations, RPM has been linked to reduced hospitalization rates and improved chronic disease control.
Some facilities now operate centralized “command hubs,” where technicians review incoming data streams and escalate only clinically relevant alerts , minimizing noise while preserving vigilance.
Impact:
Hospital at Home programs rely heavily on remote patient monitoring systems. After discharge, patients recovering from surgery or acute illness can be monitored using FDA-approved devices that track heart rate, oxygen saturation, glucose levels, and mobility patterns.
Clinicians access real-time data integrated into electronic health records, allowing them to intervene before complications escalate. For overstretched hospitals, this translates into better bed turnover and capacity management.
Virtual clinical trials are also increasingly built on RPM foundations, expanding recruitment diversity while improving protocol adherence.
Impact:
In emergency evacuation scenarios, natural disasters, conflict zones, or mass casualty events, monitoring continuity becomes critical.
Portable remote patient monitoring devices allow responders to transmit ECG readings, oxygen levels, and blood pressure data from the field to receiving hospitals. This ensures the receiving team is prepared before arrival.
In evacuation centers, wearable devices support triage by identifying vulnerable individuals whose vitals signal emerging distress.
Impact:
Offshore rigs, mining sites, and energy platforms often operate hours from the nearest hospital. Remote patient monitoring in industrial settings provides a safety net.
Workers can be equipped with biometric wearables tracking heart rate, oxygen saturation, and fatigue indicators. In case of an incident, clinicians onshore receive immediate patient data to guide intervention while medevac arrangements are underway.
Studies in offshore wind farms and oil platforms demonstrate that telemedical integration systems can successfully transmit real-time vitals via satellite connections, enabling timely emergency decisions.
Impact:
Residential communities, especially senior housing, are incorporating remote monitoring as part of shared healthcare infrastructure.
Motion sensors, temperature monitors, and connected scales allow caregivers or community health partners to detect early warning signs of illness or mobility decline. For elderly residents living independently, RPM extends autonomy while ensuring oversight.
In urban housing, community-level dashboards help public health officials identify disease trends and respond proactively.
Impact:
For families managing diabetes, hypertension, COPD, or heart disease, remote patient monitoring offers peace of mind.
Continuous glucose monitors, Bluetooth-enabled blood pressure cuffs, and smart scales transmit data directly to providers. Patients gain visibility into their health trends, encouraging lifestyle adjustments and medication adherence.
Research indicates that RPM is particularly effective for hypertension and congestive heart failure management, reducing hospitalizations and improving long-term outcomes.
Impact:
Cruise operators function as floating cities. When medical incidents occur at sea, evacuation may take hours.
Onboard remote patient monitoring solutions enable ship medical teams to transmit vitals, ECG readings, and ultrasound data to land-based specialists. This remote collaboration improves triage accuracy and treatment quality.
In high-density passenger environments, RPM also supports infection monitoring and outbreak management.
Impact:
Remote patient monitoring allows clinicians to access connected at-home or mobile medical devices, including blood pressure cuffs, glucometers, pulse oximeters, ECG systems, and wearables, to monitor chronic and acute conditions.
Some systems require periodic self-testing. Others operate continuously, streaming data directly into electronic health records. Bring-your-own-device models allow patients to connect smartwatches and smartphones, while enterprise-grade systems deploy dedicated FDA-cleared equipment.
As the line between monitoring and therapeutic devices evolves, regulatory oversight remains critical. Manufacturers and healthcare organizations must ensure compliance with safety, efficacy, and data protection.
Data security remains central to RPM adoption. Healthcare organizations must ensure patient data is stored in secure environments with role-based access control.
Interoperability is equally important. Integration with EHR systems, often through FHIR standards, ensures that clinicians can access continuous health status data without disrupting their workflows.
Automated analytics tools are increasingly deployed to filter signal from noise, surfacing only clinically relevant alerts.
Remote patient monitoring is no longer confined to chronic disease management. It is supporting:
For healthcare providers, RPM enables earlier intervention and stronger data-driven decisions. For organizations, it reduces operational risk and improves efficiency. For patients, it provides visibility and reassurance.
As regulatory frameworks evolve and telehealth flexibility expands, remote patient monitoring is moving from pilot programs to permanent infrastructure.
Organizations that treat RPM as a strategic capability, rather than a temporary tool, will be better positioned to manage capacity, improve outcomes, and extend care into the environments where it is most needed.Monitoring care from anywhere isn’t just a trend; it’s the future of health.
At SmartFuture, we’re laying the digital foundation for continuous, borderless care. Consult with our team and become a part of the healthcare revolution.
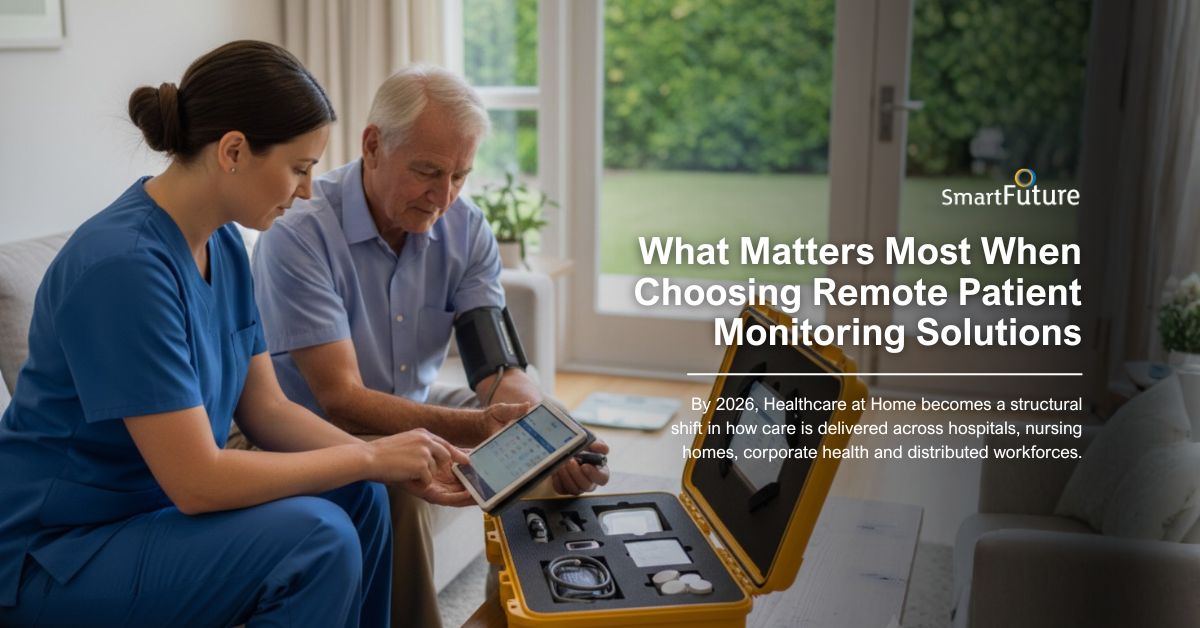
Healthcare at home is no longer an experiment. By 2026, it is a structural shift in how care is delivered...
The World Health Organization has identified remote patient monitoring as one of the healthcare delivery models with the potential to...

Remote Patient Monitoring devices (RPM) are no longer an experimental model of care. It is becoming a structural pillar of...
Follow our newsletter. We will regulary
update our latest
project and availability.

OurSmartFuture is a healthcare technology company specializing in white-label remote patient monitoring solutions for hospitals, clinics, and healthcare organizations worldwide. We help providers extend care beyond traditional settings through secure, scalable patient remote monitoring systems designed for modern healthcare delivery.
© 2026 SmartFuture - All Rights Reserved