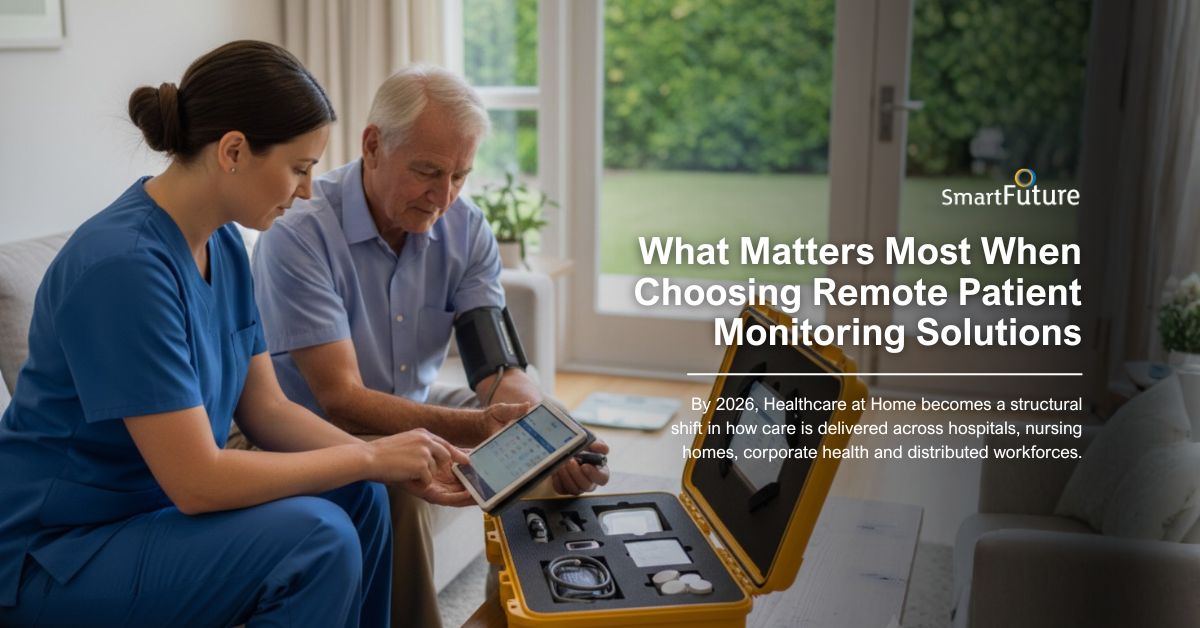
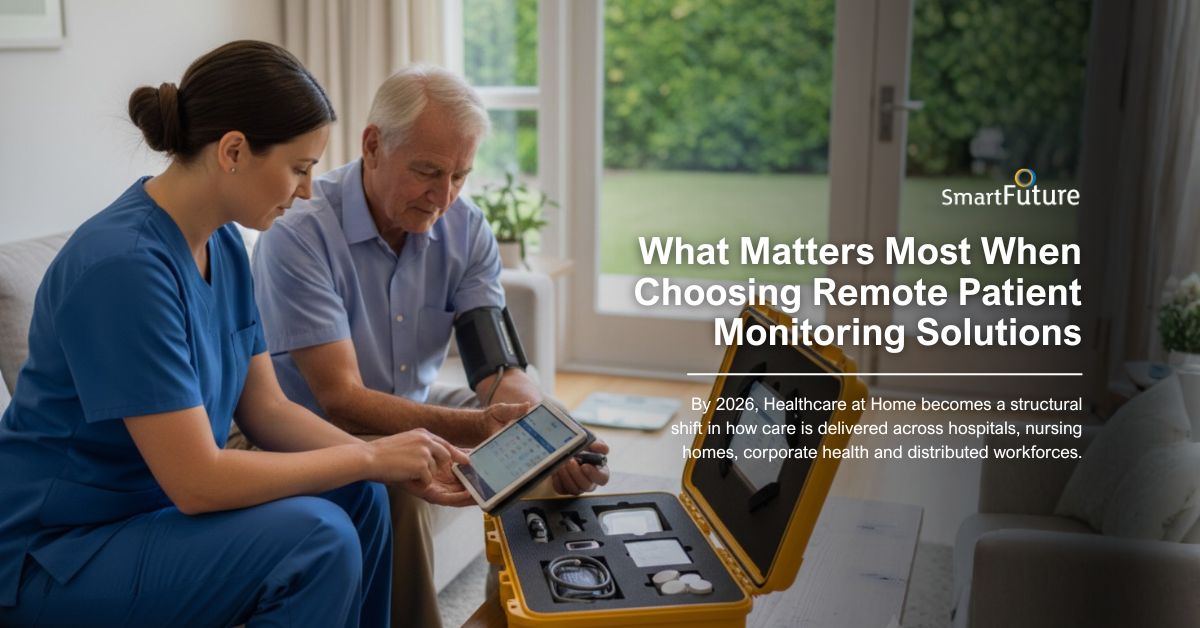
Healthcare at home is no longer an experiment. By 2026, it is a structural shift in how care is delivered across hospitals, nursing homes, corporate health programs, insurers, and distributed workforces. Remote patient monitoring solutions now sit at the center of this transformation. They are not simply devices collecting vitals; they are operational infrastructure powering early detection, resource efficiency, and value-based care.
The global patient monitoring market is projected to approach $80 billion by 2029, growing at nearly 12% annually. That growth is not driven by hype. It is driven by outcomes: fewer emergency transfers, earlier deterioration detection, improved capacity management, and better use of clinical staff.
For decision-makers, the stakes are high. Choosing the right remote patient monitoring solution strengthens your healthcare at home strategy. Choosing poorly results in unused hardware, fragmented data, workflow friction, and long-term cost overruns.
At SmartFuture, we believe the conversation in 2026 must move beyond device features. The real question is: Does your remote patient monitoring system strengthen your organization’s long-term care model?
Here is what matters most.
Start with the most fundamental question: Can the system detect patient deterioration early enough to intervene?
Marketing claims are not enough. You need real-world implementation data.
In acute settings, studies show that nearly 80% of ICU transfers occur within 48 hours of admission. Continuous monitoring systems that identify risk 18 hours before intervention create a measurable advantage. That window allows clinicians to prevent crises rather than respond to them.
In post-acute and healthcare at home environments, deterioration is slower and more subtle. Systems must establish patient baselines and detect gradual changes over three to five days. Continuous monitoring in home-based care settings is not about alarm volume, it is about intelligent trend recognition.
Detection accuracy must be paired with appropriate early warning thresholds tailored to your care environment.
Most healthcare organizations operate in complex IT ecosystems. Electronic health records, billing systems, analytics platforms, and device fleets often operate in silos.
A modern remote patient monitoring solution must integrate seamlessly into your existing infrastructure, not through manual uploads or temporary workarounds, but through fully functioning interoperability.
Ask vendors to demonstrate:
Data should move automatically from device capture to clinician dashboards without duplication or delay.
When integration works, clinical teams focus on care instead of acting as data intermediaries.
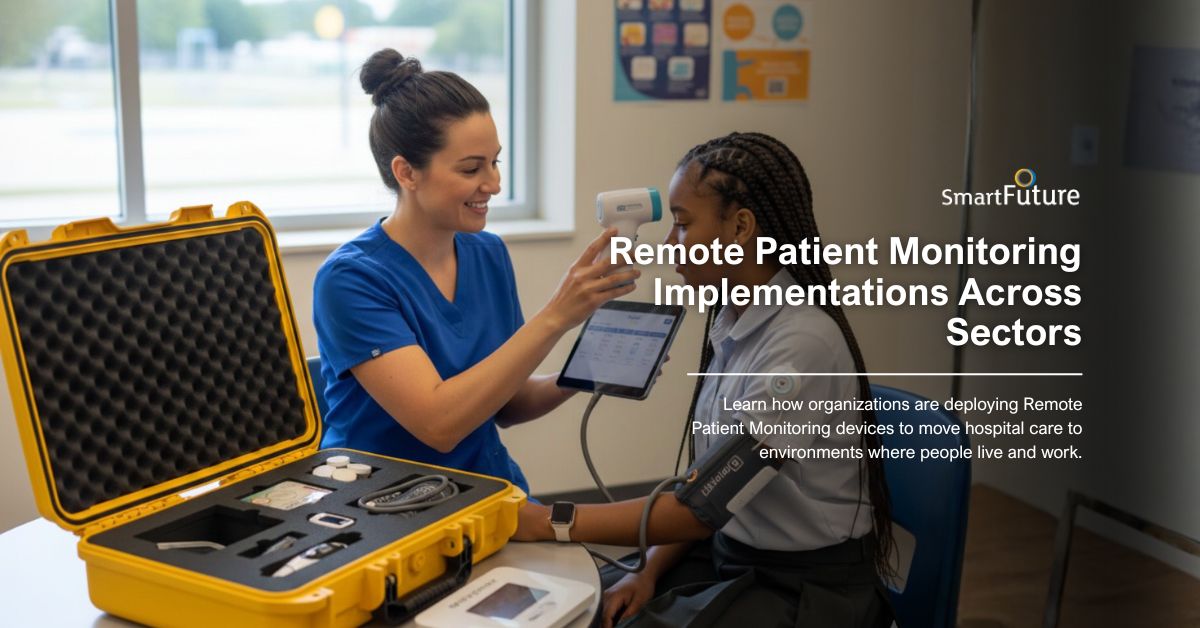
Healthcare at home is not a single use case.
An emergency department requires different alert sensitivity compared to a rehabilitation facility. A nursing home serving elderly residents with chronic disease requires different baseline modeling compared to a post-surgical recovery program.
Your remote patient monitoring system must allow configuration by:
One-size-fits-all alert settings create alarm fatigue or missed deterioration. Flexibility is essential.
Adoption determines return on investment. If clinicians find the system complicated or intrusive, usage declines. If patients struggle with devices, compliance drops and data quality suffers.
User-centered design in 2026 means:
Mobile access is particularly critical. Healthcare at home demands mobility. Clinicians must review alerts across distributed environments, not just at fixed stations.
Deployment is not the end of the journey.
Healthcare systems evolve. Staff turnover occurs. Regulations change. Patient populations shift. A strong remote patient monitoring partner provides:
Vendors who disappear after installation create operational risk. RPM is a five- to ten-year investment. Your partner must be prepared for that timeline.
Healthcare at home expands the attack surface for cybersecurity threats.
In the United States, FDA clearance is mandatory for medical device commercialization. HIPAA compliance governs patient data protection. In Europe, CE marking and MDR compliance are non-negotiable, alongside GDPR data standards.
Beyond regulatory minimums, organizations should request:
Patient data must remain secure, exportable, and fully under your control.
A pilot program is not a strategy.
Many monitoring solutions perform well in small trials but struggle at scale. Your system must support:
Scalability is not theoretical. Ask vendors for real examples of sustained, full-scale implementations.
Healthcare organizations lose billions annually to supply chain inefficiencies and vendor misalignment.
The lowest upfront cost rarely produces the lowest long-term cost.
Evaluate:
Calculate five-year total cost of ownership. Factor in staff efficiency gains and reduced hospitalizations when modeling ROI.
In 2026, differentiation matters.
Healthcare providers, insurers, and enterprise health programs increasingly demand ownership over the patient experience. A white-label remote patient monitoring solution allows organizations to:
White-label RPM solutions are not cosmetic changes. They create strategic leverage.
For hospital systems, white-label deployment reinforces brand equity in healthcare at home programs. For insurers, it strengthens customer engagement. For corporate health providers, it ensures continuity with existing digital platforms.
At SmartFuture, our white-label architecture allows organizations to integrate RPM seamlessly into their existing digital ecosystem without sacrificing brand integrity or operational control.
Ownership of the patient journey matters. White-label solutions make that possible.
Technology cannot fix broken workflows.
Before selecting a remote patient monitoring solution, map:
Define what improvement looks like before deployment. Align RPM capabilities with operational goals.
Implementation requires buffer time. Change management cannot be rushed. Identify internal champions and plan for staff training cycles.
Healthcare at home is a transformation initiative — not a plug-and-play software purchase.
Healthcare at home in 2026 demands more than remote devices.
It demands intelligent detection, seamless integration, secure data infrastructure, scalable architecture, strong vendor partnership, and strategic brand control through white-label deployment.
The right remote patient monitoring solution becomes invisible. It surfaces actionable insights, reduces friction, and strengthens care delivery without increasing workload.
The wrong solution becomes expensive shelfware.
Start with your goals. Evaluate beyond the sales pitch. Verify real-world performance. Confirm integration. Demand compliance documentation. Calculate total cost of ownership. Prioritize scalability. And choose a partner aligned with your long-term vision.
Choosing the right remote patient monitoring solution and direct home medical kit is a strategic move that shapes your care delivery model for years to come.
At SmartFuture, we help healthcare providers, nursing homes, hospitals, insurers, and enterprise organizations deploy scalable RPM infrastructure and integrated home medical kits that work in real-world environments. From white-labeled remote monitoring platforms to rugged, ready-to-deploy MediKit solutions, we ensure your organization gains clinical visibility, operational efficiency, and brand control — without unnecessary complexity.
If you’re building a Healthcare at Home program, expanding remote care services, or strengthening distributed medical response, our team will guide you through:
Connect with SmartFuture today and explore how our RPM platform and Direct Home Medical Kit solutions can support your organization’s next stage of growth.
Healthcare at home is no longer an experiment. By 2026, it is a structural shift in how care is delivered...
The World Health Organization has identified remote patient monitoring as one of the healthcare delivery models with the potential to...

Remote Patient Monitoring devices (RPM) are no longer an experimental model of care. It is becoming a structural pillar of...
Follow our newsletter. We will regulary
update our latest
project and availability.

OurSmartFuture is a healthcare technology company specializing in white-label remote patient monitoring solutions for hospitals, clinics, and healthcare organizations worldwide. We help providers extend care beyond traditional settings through secure, scalable patient remote monitoring systems designed for modern healthcare delivery.
© 2026 SmartFuture - All Rights Reserved